Abstract
Introduction: The treatment of acute myeloid leukaemia (AML) with intensive induction regimens remains a challenge in low and middle incomes countries. Early induction related deaths particularly due to infectious complications are a major problem. This is in stark contrast to high-income countries where induction mortality has declined significantly over the last 2 decades with improved antibiotic use and supportive care. In this study we assess induction mortality (all cause and infection related) in AML patients who received intensive induction therapy in a tertiary cancer centre in India over a 10-year period (2008-2017).
Methods: We included patients with newly diagnosed AML treated at Cancer Institute, Chennai in South India who received intensive induction therapy. Intensive therapy was defined as use of any anthracycline with cytarabine (3+7/ADE/others). We assessed baseline demographics including age, gender, cytogenetic risk status, and type of induction regimen used. We also assessed key clinical outcomes including patterns of antimicrobial prophylaxis and treatment, infectious complications, cause of death, ICU stay, and length of hospital stay. Induction mortality was defined as deaths occurring within 45 days of initiating treatment for AML or start of 2nd induction.
Results: Between January 2008 and December 2017, 510 patients with AML were evaluated at Cancer Institute, Chennai and accepted for treatment. Excluding 51 patients with APML and 55 patients who were unfit for intensive induction, 404 patients received treatment with an intensive induction regimen. Median age was 23 years (Range: 1-74 years) and 219 (54.2%) were male patients. 165(40.8%) patients were less than 18 years of age. Among those who had cytogenetic and/ molecular data for risk stratification [N=341 (84.7%)], 101 (29.6%) were low risk, 166 (48.7%) intermediate risk and 74 (21.7%) high risk. Therapy details: 318 (78.7%) patients received daunorubicin and cytarabine ('3+7'), 52 (12.9%) received ADE, and 38 (8.4%) received other combinations ofdaunorubicin and cytarabine.
87(21.5%) of the cases had infection at the time of presentation. 389(96.8%) had an episode of febrile neutropenia with 184(45.5%) requiring management in Intensive Care Unit (ICU). Focus of infection could be identified in 294(72.7%) of the patients with 207(51.2%) having a positive culture.
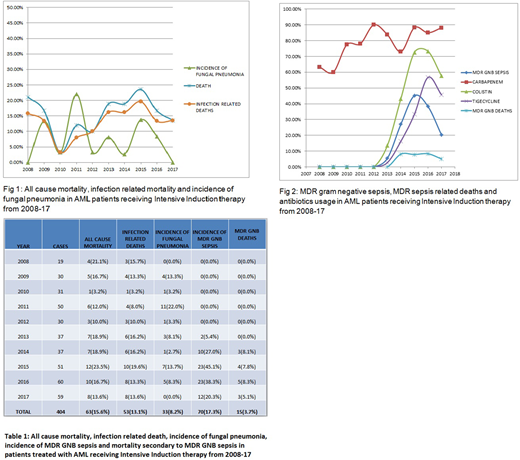
The overall incidence of induction mortality over the entire study period was 15.6%(n=63)and 14.8% for the most recent year included (2017). The majority of the deaths (n=53; 84.1%) were due to infectious complications (fig1). Median time to death from start of induction was 19 days. The incidence of fungal pneumonia significantly reduced since 2012 when thethe antifungal prophylaxis was switched from fluconazole to voriconazole (p=0.03). Starting in 2012, an increase in the incidence of multi-drug resistance (MDR) gram negative septicaemia and mortality (MDR: carbapenem resistant enterobacteriacea
sensitive only to colistin and tigecycline) was noted. This led to proactive use of colistin in patients with febrile neutropenia and septic shock, a GI focus or baseline stool colonisation by MDR gram negative organisms.Despite this, during the last 4 years(2014-2017), there has been a significant rise in the incidence of sepsis and death due to MDR gram negative organisms (fig2). The proportion of deaths attributable to MDR sepsis is 23.8%. The early use of colistin, tigecycline and carbapenems did not significantly decrease the mortality.
Conclusions: The induction mortality remains high at 15.6% and is in contrast to the declining induction mortality in high-income countries. While the morbidity and mortality due to specific infections (specifically fungal pneumonia) have changed over time, there is no signfiicant decline in infectious or all cause induction mortality over the 10 years. In the last four years, MDR gram negative sepsis has been a major cause of morbidity and mortality. The early and increased use of broad spectrum antibiotics like tigecycline, colistin and carbapenems has not led to a decrease in MDR gram negative sepsis. Overall, despite improvements in supportive care and early use of broad spectrum antimicrobial agents, infection related morbidity and mortality remains a substantial challenge in treating acute myeloid leukaemia in low- and middle-income countries.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal